Op-Ed

Op-Ed
Active and healthy cities?
No time to read? La Fabrique de la Cité has got you covered. Check our newsletter #54.
To be informed of our upcoming publications, please subscribe to our newsletter and follow our Twitter and LinkedIn accounts.
Find this publication in the project:
These other publications may also be of interest to you:

Op-Ed
Death and life of CBD

Op-Ed
Is resilience useful?

Op-Ed
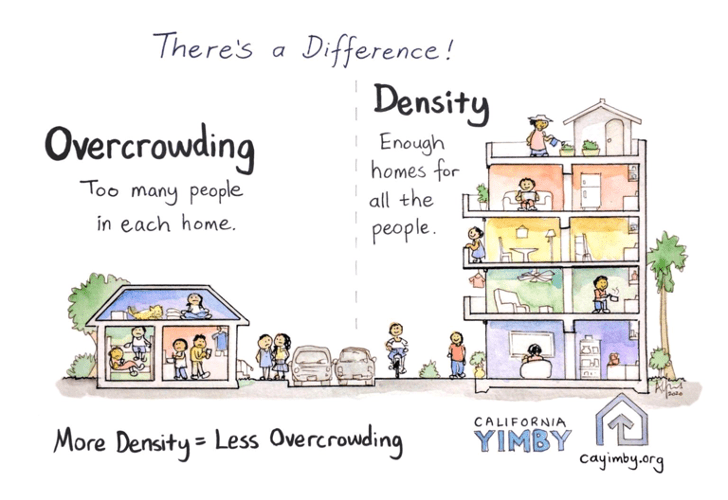
Long live urban density!
Issue brief
Behind the words: Recovery

Op-Ed
Sending out an SOS
Op-Ed
The ideal culprit
Issue brief
Behind the words: density

Issue brief
Behind the words: telecommuting

Issue brief
Behind the words: urban congestion

Issue brief
Behind the words: food security

Op-Ed
180° Turn

Op-Ed
Cities in safe boot mode
Op-Ed
Across cities in crisis

Op-Ed
A street named desire
Actualité
Resilience: an operational concept?

Expert viewpoint
Zoé Vaillant: health inequalities are rooted in local areas

Expert viewpoint
Viktor Mayer-Schönberger: what role does big data play in cities?

Expert viewpoint
Thomas Madreiter: Vienna and the smart city
La Fabrique de la Cité
La Fabrique de la Cité is a think tank dedicated to urban foresight, created by the VINCI group, its sponsor, in 2010. La Fabrique de la Cité acts as a forum where urban stakeholders, whether French or international, collaborate to bring forth new ways of building and rebuilding cities.